A well-done trial comparing showed the steroid doesn't improve pain or function scores, and may increase cartilage breakdown. Does this spell the end of the practice? F. Perry Wilson, MD, breaks down the data in 150 seconds.
Steroid injections for osteoarthritis is like Snapchat. Everyone seems to be doing it, and no one is quite sure why.
But a major blow to that most common – and lucrative – of in-office procedures was dealt this week, in the form of this trial, appearing in the Journal of the American Medical Association.
Far from the shot in the arm – knee – the good makers of triamcinolone injection needed, this trial shows that the steroid shot may be no better than saline, and actually might be a bit worse.
By way of background, the use of steroid injections for osteoarthritis has always been a bit controversial. The most recent Cochrane review of the literature on the subject, conducted in 2015, found a modest benefit to the practice, but cautioned:

Their forest plot, pictured here, shows the results of 25 trials.
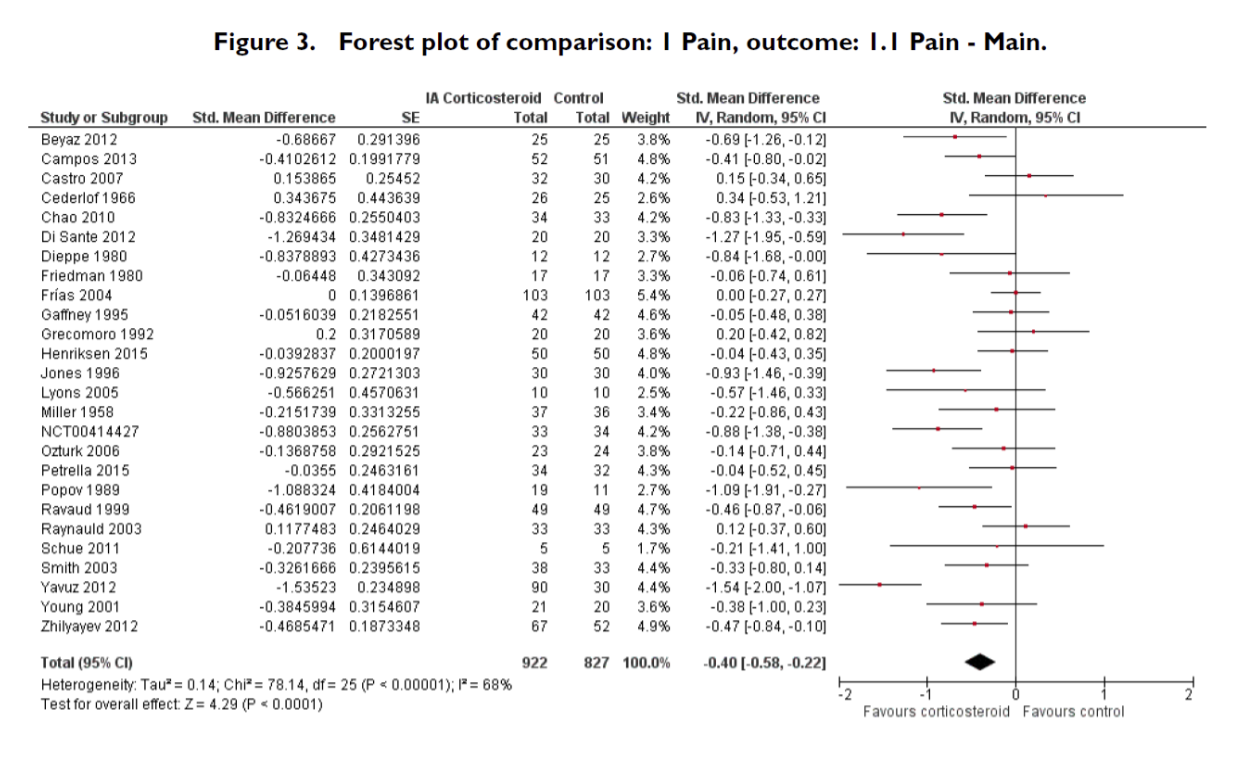
The effects are all over the place. And most trials were seriously underpowered.
The current study may be the best of the bunch. Researchers randomized 140 patients with knee osteoarthritis to steroid or saline injection every 12 weeks for 2 years. At each visit, they asked about pain and function. At baseline, 1 year, and 2 years in, they also got a knee MRI to examine the cartilage.
These patients were well-selected. They not only had osteoarthritis but evidence of synovitis on ultrasound. In other words, if anyone is going to respond to steroids, this is the group.
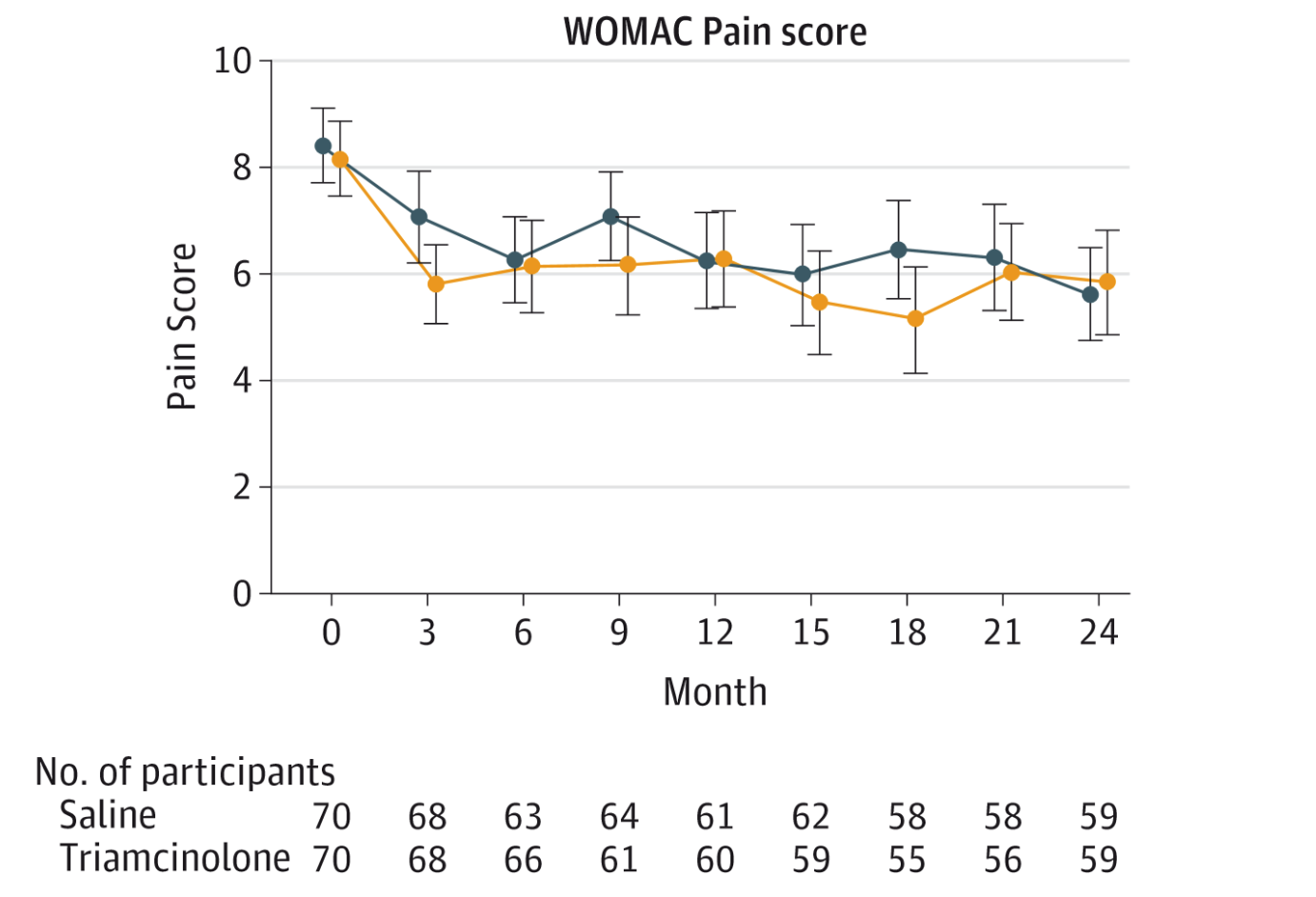
And you know where this is going. There was no difference in knee pain at any time point across the two groups, though pain did decrease a bit in all patients. Thank you, placebo effect. No changes in function, stiffness or walk time, either.
In fact the only thing that changed significantly between the groups was the change in cartilage thickness. Those who got steroid lost 0.16mm more cartilage than those who got saline, a statistically significant if clinically indeterminate result.
Do steroids still have a role? I spoke with an orthopedic surgeon who pointed out that steroids should really only be used for flares of osteoarthritis, not as a long-term treatment strategy. He also mentioned that the pain relief is real, but short-lived, and may not have been captured by the every-3-month pain surveys the researchers conducted.
But with this trial showing potential cartilage loss, and somewhat shoddy older data, it's hard to justify the procedure without citing anecdotal evidence. Hyaluronic acid injections, look out. You might be the next to feel the pinch.
, is an assistant professor of medicine at the Yale School of Medicine. He is a �������� reviewer, and in addition to his video analyses, he authors a blog, . You can follow .
